Your posture is one of the first things other people notice about you and can affect so much more in your life than just spinal health. Healthy posture has been linked to better respiratory health and has even been shown to affect your confidence. In this article, we explore a few other surprising facts about posture.
Ideal posture doesn’t mean having a straight back.
Many people think having good posture means standing as straight as possible with your shoulders pulled back. This is actually a relatively unnatural posture and requires a lot of energy to maintain. Ideal posture, where the spine rests in its most comfortable and strongest position, is where the neck has a gentle curve backwards, the thoracic is curved gently forwards and the lower back curves back again. These curves create an elongated ‘S’ shape and can be seen when viewing a person from side on.
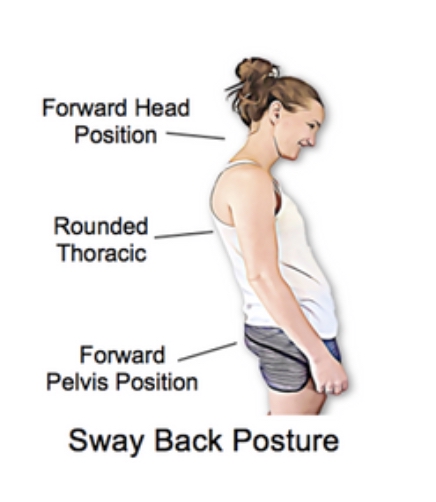
There are four common postural patterns other than ‘ideal posture’.
For those who don’t have ideal posture, four common variations are seen, these are; kyphosis (excessive curve of the thoracic region), lordosis (excessive curve of the lower back), flat back (loss of the normal spinal curves) and sway back (where the pelvis is pushed in front of your centre of gravity and the upper body leans back to compensate). Each of these postures is often accompanied by a typical pattern of joint and muscle stiffness that can lead to pain and injury. Your physiotherapist is able to assess your posture and identify any ways this may be contributing to your pain. They can also help you to change your posture with strategies to increase spinal mobility and strength.
Regular movement is just as important as your posture.
While ideal posture has been shown to reduce the amount of stress and tension found in the spinal muscles, holding yourself rigidly in one position is also not healthy. Ideally, our spines will be flexible and able to move through their full range without pain or stiffness. Regular movement is the key to healthy joints, including the spine. If you finding yourself sitting or standing for long periods, try to find time to stretch as well as working on your posture.
Posture can affect your ability to breathe
Your ribs are attached to the 12 thoracic vertebrae in the thoracic region of the spine. When this part of the spine is bent forwards (this is called a kyphosis) the ribs are unable to move as freely. This can impact your ability to breathe to full capacity if the thoracic spine is help permanently in this posture. In extreme cases this can affect overall health and well being as well as contribute to neck and lower back pain.
Your physiotherapist is able to provide advice and exercises to help you improve your posture based on your individual habits, muscle strength and length.