CUMBERLAND PHYSIOTHERAPY PARRAMATTA:
Cauda equina syndrome is a rare condition that you may not have heard of, however it can have catastrophic consequences if it is not recognised and treated quickly. This condition occurs in up to two percent of cases of herniated lumbar discs, causing loss of lower leg function, incontinence and lower back pain. It is one of the few medical emergencies related to back pain and can be devastating if symptoms persist.
What Causes Cauda Equina Syndrome?
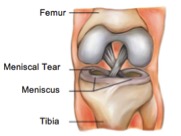
At the end of the spinal cord, there is a bundle of spinal nerves arranged in a formation that resembles a horse’s tail. (In Latin, cauda equina means “horse’s tail”.) These nerves are housed within the spinal canal in the lumbar region.
If, for any reason, these nerves become compressed, signals to the bowel, bladder, and lower limbs can be disrupted. Left untreated, this compression can result in permanent paraplegia and incontinence. Common causes of compression include disc herniation due to disc degeneration, tumours, inflammatory disorders, spinal stenosis, or complications following surgery. Trauma-related caudaequina syndrome—such as from knife wounds or motor vehicle accidents—can affect people of all ages.
Signs and Symptoms
This syndrome can be difficult to diagnose because its symptoms mimic those of many other conditions. However, there are certain warning signs that health professionals are trained to take very seriously.
These include:
Sudden loss of reflexes in the legs Unusual and rapid onset of bladder or bowel incontinence, or sexual dysfunction Pain in one or both legs Motor and sensory loss Tingling or numbness in the saddle region (groin and inner thighs) Bilateral sciatica
These symptoms are often associated with severe lower back pain. If you suddenly experience more than one of these symptoms—particularly incontinence—seek immediate medical attention.
Treatment Options
Treatment will depend on the severity and underlying cause of the syndrome. However, in most cases, cauda equina syndrome requires urgent decompression surgery to relieve pressure on the affected nerves. The longer the delay between symptom onset and surgery, the lower the chances of a full recovery.
Most patients will require physiotherapy, pain management, and psychological support—even if treatment is delivered promptly. While this is a very rare condition, public awareness is essential, as early intervention is crucial to prevent permanent damage.
None of the information in this article is a substitute for medical advice. Always consult a qualified health professional regarding your specific condition.